
Meet the Researchers
Our passionate JDRF-funded researchers in Canada work collaboratively at the cutting-edge of research to cure and improve the lives of those living with type 1 diabetes (T1D).
Every year, JDRF funds researchers in Canada, and globally with our affiliate partners, whose research aims to either find cures for T1D or improve the lives today for people living with the disease.
Our researchers are passionate about what they do. We work collaboratively with them to leverage their knowledge, creativity and diverse expertise to accelerate our global research strategy, via roadmaps designed to bring us efficiently towards a world without T1D.
Learn more about how our researchers are collaborating on cure research and improving the lives of those people living with T1D
Cure Research
 Dr. Yi-Chun Chen (BC) is a postdoctoral fellow working in Dr. Bruce Verchere’s laboratory at the University of British Columbia. She earned her PhD in cellular and integrative physiology from Indiana University School of Medicine in the United States. Her research focuses on the causes and consequences of insufficient islet prohormone processing in diabetes.
Dr. Yi-Chun Chen (BC) is a postdoctoral fellow working in Dr. Bruce Verchere’s laboratory at the University of British Columbia. She earned her PhD in cellular and integrative physiology from Indiana University School of Medicine in the United States. Her research focuses on the causes and consequences of insufficient islet prohormone processing in diabetes.
 Dr. Jayne Danska (ON) holds the Anne and Max Tanenbaum Chair in Molecular Medicine and is a professor at the University of Toronto Faculty of Medicine and a senior scientist at The Hospital for Sick Children.. She is studying the role of the community of microbes that inhabit the human intestine (the microbiome) in altering risk for, and the progression of, T1D. The ultimate objective of her work is to identify new therapeutics to prevent the disease.
Dr. Jayne Danska (ON) holds the Anne and Max Tanenbaum Chair in Molecular Medicine and is a professor at the University of Toronto Faculty of Medicine and a senior scientist at The Hospital for Sick Children.. She is studying the role of the community of microbes that inhabit the human intestine (the microbiome) in altering risk for, and the progression of, T1D. The ultimate objective of her work is to identify new therapeutics to prevent the disease.
 Dr. Jan Dutz (BC) is an Investigator at BC Children’s Hospital and a professor in the Faculty of Medicine at the University of British Columbia. He is leading a phase 2/3 clinical trial testing whether a disease-modifying drug called ustekinumab can slow progression of T1D in young adults recently diagnosed. Ustekinumab – which is already approved to treat psoriasis and inflammatory bowel disease – previously showed promise in a JDRF-funded pilot trial conducted by Dr. Dutz and his team.
Dr. Jan Dutz (BC) is an Investigator at BC Children’s Hospital and a professor in the Faculty of Medicine at the University of British Columbia. He is leading a phase 2/3 clinical trial testing whether a disease-modifying drug called ustekinumab can slow progression of T1D in young adults recently diagnosed. Ustekinumab – which is already approved to treat psoriasis and inflammatory bowel disease – previously showed promise in a JDRF-funded pilot trial conducted by Dr. Dutz and his team.
 Dr. Timothy Kieffer (BC) is a professor in the Department of Cellular and Physiological Sciences and the Department of Surgery at the University of British Columbia. He was one of the first researchers in the world to show that human stem cells can be differentiated into glucose-responsive insulin-producing cells. The procedure he developed set the stage for clinical trials now in progress, and Dr. Kieffer and his team continue to work on refining approaches to cell replacement using this approach. With continued investment, such approaches could one day reduce or eliminate the need for daily insulin injections.
Dr. Timothy Kieffer (BC) is a professor in the Department of Cellular and Physiological Sciences and the Department of Surgery at the University of British Columbia. He was one of the first researchers in the world to show that human stem cells can be differentiated into glucose-responsive insulin-producing cells. The procedure he developed set the stage for clinical trials now in progress, and Dr. Kieffer and his team continue to work on refining approaches to cell replacement using this approach. With continued investment, such approaches could one day reduce or eliminate the need for daily insulin injections.
 Dr. Gregory Korbutt (AB) is a professor of surgery at the University of Alberta. He is using different techniques to safeguard cells with the goal of developing a more accessible source of insulin-producing tissue for transplantation into patients with T1D. Dr. Korbutt and his team are using their new 3D ‘scaffolding’ technology to make islet transplants more widely available and functional.
Dr. Gregory Korbutt (AB) is a professor of surgery at the University of Alberta. He is using different techniques to safeguard cells with the goal of developing a more accessible source of insulin-producing tissue for transplantation into patients with T1D. Dr. Korbutt and his team are using their new 3D ‘scaffolding’ technology to make islet transplants more widely available and functional.
 Dr. Megan Levings (BC), of the University of British Columbia and BC Children's Hospital Research Institute is one of Canada’s leading immunologists. She holds two JDRF grants: one enables collaboration testing samples from a clinical trial of a drug called ustekinumab to understand how the drugs works in people with T1D. The other is a CIHR-JDRF grant that is applying novel approaches to better understand the causes of T1D and development of cellular therapies to cure the disease.
Dr. Megan Levings (BC), of the University of British Columbia and BC Children's Hospital Research Institute is one of Canada’s leading immunologists. She holds two JDRF grants: one enables collaboration testing samples from a clinical trial of a drug called ustekinumab to understand how the drugs works in people with T1D. The other is a CIHR-JDRF grant that is applying novel approaches to better understand the causes of T1D and development of cellular therapies to cure the disease.
 Dr. Dan Luciani (BC) is an associate professor at the University of British Columbia and an investigator at BC Children’s Hospital. Through a JDRF-funded innovation grant, he will examine how the mitochondria impacts the development of stem cell-derived beta cells for transplantation.
Dr. Dan Luciani (BC) is an associate professor at the University of British Columbia and an investigator at BC Children’s Hospital. Through a JDRF-funded innovation grant, he will examine how the mitochondria impacts the development of stem cell-derived beta cells for transplantation.
 Dr. Francis Lynn (BC) is an associate professor in the Faculty of Medicine at the University of British Columbia and an investigator at BC Children’s Hospital. Dr. Lynn’s team is working towards developing a cure for T1D by replacing insulin-producing beta cells via transplantation. His work focuses on the genetic mechanisms that regulate the formation of islet beta cells from stem cells or progenitor cells.
Dr. Francis Lynn (BC) is an associate professor in the Faculty of Medicine at the University of British Columbia and an investigator at BC Children’s Hospital. Dr. Lynn’s team is working towards developing a cure for T1D by replacing insulin-producing beta cells via transplantation. His work focuses on the genetic mechanisms that regulate the formation of islet beta cells from stem cells or progenitor cells.
 Dr. Hongshen Ma (BC) is an associate professor in the School of Biomedical Engineering at University of British Columbia. Through a JDRF-funded innovation grant, he will develop a new technology to measure insulin secretion capability of stem cell-derived beta cells for the purpose of optimizing functionality of these cells.
Dr. Hongshen Ma (BC) is an associate professor in the School of Biomedical Engineering at University of British Columbia. Through a JDRF-funded innovation grant, he will develop a new technology to measure insulin secretion capability of stem cell-derived beta cells for the purpose of optimizing functionality of these cells.
 Dr. Patrick MacDonald's (AB) research focuses on understanding the factors that control insulin production by islet cells. Human insulin production is impacted by factors such as nutrition, genetics, and exposure to environmental chemicals. MacDonald and his team are cataloging the variability in human insulin secretion, islet cell functions, and molecular profiles across many pancreas organ donors with and without diabetes in order to better understand the cellular functions of insulin-producing islet cells. This research will create a comprehensive ‘encyclopedia’ that will be available to researchers around the world, supporting a better understanding of human insulin secretion and diabetes.
Dr. Patrick MacDonald's (AB) research focuses on understanding the factors that control insulin production by islet cells. Human insulin production is impacted by factors such as nutrition, genetics, and exposure to environmental chemicals. MacDonald and his team are cataloging the variability in human insulin secretion, islet cell functions, and molecular profiles across many pancreas organ donors with and without diabetes in order to better understand the cellular functions of insulin-producing islet cells. This research will create a comprehensive ‘encyclopedia’ that will be available to researchers around the world, supporting a better understanding of human insulin secretion and diabetes.
 Dr. Despoina Manousaki (QC) is a pediatric endocrinologist at CHU Sainte-Justine Research Centre and assistant professor at Université de Montréal. Dr. Manousaki’s research focuses on the genetics of complex disease in childhood. Her team uses genomics, bioinformatics, and genetic epidemiology methods to better understand the genetic architecture of complex disease, and to apply these findings in translational research.
Dr. Despoina Manousaki (QC) is a pediatric endocrinologist at CHU Sainte-Justine Research Centre and assistant professor at Université de Montréal. Dr. Manousaki’s research focuses on the genetics of complex disease in childhood. Her team uses genomics, bioinformatics, and genetic epidemiology methods to better understand the genetic architecture of complex disease, and to apply these findings in translational research.
 Dr. Andras Nagy (ON) is a senior investigator at the Lunenfeld–Tanenbaum Research Institute at Mount Sinai Hospital in Toronto and a Canada Research Chair in Stem Cells and Regeneration. Dr. Nagy’s research focusses on novel approaches to generating human stem cells and creating genomic technologies to harness the potential of stem cells. His two patented technologies – FailSafe™ and “immunocloaking” strategy – contribute to his ongoing research on the functionality and safety of insulin-producing islet cell transplants from human stem cells.
Dr. Andras Nagy (ON) is a senior investigator at the Lunenfeld–Tanenbaum Research Institute at Mount Sinai Hospital in Toronto and a Canada Research Chair in Stem Cells and Regeneration. Dr. Nagy’s research focusses on novel approaches to generating human stem cells and creating genomic technologies to harness the potential of stem cells. His two patented technologies – FailSafe™ and “immunocloaking” strategy – contribute to his ongoing research on the functionality and safety of insulin-producing islet cell transplants from human stem cells.
 Dr. Maria Cristina Nostro (ON) is a Senior Scientist at the McEwen Stem Cell Institute at University Health Network and Associate Professor at the University of Toronto. Dr. Nostro holds a JDRF-CIHR grant which supports she and her team to pursue work that will use new transplantation strategies and apply universal donor stem cells to develop a superior islet-like product for people with T1D that will require little or no immunosuppression.
Dr. Maria Cristina Nostro (ON) is a Senior Scientist at the McEwen Stem Cell Institute at University Health Network and Associate Professor at the University of Toronto. Dr. Nostro holds a JDRF-CIHR grant which supports she and her team to pursue work that will use new transplantation strategies and apply universal donor stem cells to develop a superior islet-like product for people with T1D that will require little or no immunosuppression.
 Dr. Amanda Oakie (ON) is a postdoctoral fellow in Dr. Cristina Nostro’s lab at the McEwen Stem Cell Institute, University Hospital Network in Toronto. Dr. Oakie’s research examines methods to improve the yield obtained from beta-like cells derived from human pluripotent stem cells. Her work examines different strategies to expand the beta-like cells throughout differentiation.
Dr. Amanda Oakie (ON) is a postdoctoral fellow in Dr. Cristina Nostro’s lab at the McEwen Stem Cell Institute, University Hospital Network in Toronto. Dr. Oakie’s research examines methods to improve the yield obtained from beta-like cells derived from human pluripotent stem cells. Her work examines different strategies to expand the beta-like cells throughout differentiation.
 Dr. Andrew Pepper (AB) is an assistant professor in the Division of Surgical Research at the University of Alberta who formerly trained with Dr. James Shapiro. Along with his team, he is examining the underlying mechanisms that govern pancreatic beta cell survival and function, with the ultimate goal of developing islet replacement therapies that could become a universal treatment for a broader range of people living with T1D.
Dr. Andrew Pepper (AB) is an assistant professor in the Division of Surgical Research at the University of Alberta who formerly trained with Dr. James Shapiro. Along with his team, he is examining the underlying mechanisms that govern pancreatic beta cell survival and function, with the ultimate goal of developing islet replacement therapies that could become a universal treatment for a broader range of people living with T1D.
 Dr. Elizabeth Rideout (BC) is an associate professor at the University of British Columbia. Dr. Rideout’s research investigates the effect of biological sex on metabolic genes and pathways. Her team will apply this work to T1D by examining how beta cell dysfunction differs between males and females during the progression of T1D. Her research will inform prevention and treatment strategies that account for the impact of biological sex.
Dr. Elizabeth Rideout (BC) is an associate professor at the University of British Columbia. Dr. Rideout’s research investigates the effect of biological sex on metabolic genes and pathways. Her team will apply this work to T1D by examining how beta cell dysfunction differs between males and females during the progression of T1D. Her research will inform prevention and treatment strategies that account for the impact of biological sex.
 Dr. Rangarajan Sambathkumar (ON) is a postdoctoral fellow in Dr. Nostro’s lab researching islet transplantation and universal donor stem cell-based therapies. Dr. Sambathkumar’s work involves the use of genome engineering to improve approaches for making insulin-producing beta cells from human stem cells, for cell replacement therapy in T1D.
Dr. Rangarajan Sambathkumar (ON) is a postdoctoral fellow in Dr. Nostro’s lab researching islet transplantation and universal donor stem cell-based therapies. Dr. Sambathkumar’s work involves the use of genome engineering to improve approaches for making insulin-producing beta cells from human stem cells, for cell replacement therapy in T1D.
 Dr. Robert Screaton (ON) is a senior scientist at the Sunnybrook Research Institute in Toronto. Dr. Screaton researches strategies to maximize survival of beta cells and identify genes that help the beta cells survive and function. His work promotes beta cell survival, not only during stem cell-derived transplant scenarios, but also to prevent beta cell loss that triggers T1D in the first place.
Dr. Robert Screaton (ON) is a senior scientist at the Sunnybrook Research Institute in Toronto. Dr. Screaton researches strategies to maximize survival of beta cells and identify genes that help the beta cells survive and function. His work promotes beta cell survival, not only during stem cell-derived transplant scenarios, but also to prevent beta cell loss that triggers T1D in the first place.
 Dr. Michael Sefton (ON) is a professor at the University of Toronto Institute of Biomedical Engineering. Dr. Sefton and his team explore new ways for insulin-producing cells to be transplanted into people living with T1D. Their research examines ways to engineer tissues so that transplanted insulin-producing cells are not rejected by the immune response. Dr. Sefton’s recent research is examining the skin as a site for islet cell transplantation.
Dr. Michael Sefton (ON) is a professor at the University of Toronto Institute of Biomedical Engineering. Dr. Sefton and his team explore new ways for insulin-producing cells to be transplanted into people living with T1D. Their research examines ways to engineer tissues so that transplanted insulin-producing cells are not rejected by the immune response. Dr. Sefton’s recent research is examining the skin as a site for islet cell transplantation.
 Dr. James Shapiro, (AB) a multi-organ transplant surgeon at the University of Alberta, led the team that developed the Edmonton Protocol in the 1990s, which enabled long-lasting islet transplants in people with T1D and has been taken up by clinical centres around the world. JDRF has supported Dr. Shapiro’s work almost continuously since the 1990s. Currently, JDRF is supporting both preclinical work and clinical trials by Dr. Shapiro, in which his team is testing different approaches for disease modification and cell replacement to cure T1D.
Dr. James Shapiro, (AB) a multi-organ transplant surgeon at the University of Alberta, led the team that developed the Edmonton Protocol in the 1990s, which enabled long-lasting islet transplants in people with T1D and has been taken up by clinical centres around the world. JDRF has supported Dr. Shapiro’s work almost continuously since the 1990s. Currently, JDRF is supporting both preclinical work and clinical trials by Dr. Shapiro, in which his team is testing different approaches for disease modification and cell replacement to cure T1D.
 Dr. Peter Thompson (MB) is an assistant professor at the Max Rady College of Medicine at the University of Manitoba. Dr. Thompson’s research focuses on the heterogeneity (individual differences) of beta cells within an islet and how individual cells may respond differently to immune system attacks and stressors. His research will help determine how T1D progresses and will inform cure research aimed specifically at beta cell preservation.
Dr. Peter Thompson (MB) is an assistant professor at the Max Rady College of Medicine at the University of Manitoba. Dr. Thompson’s research focuses on the heterogeneity (individual differences) of beta cells within an islet and how individual cells may respond differently to immune system attacks and stressors. His research will help determine how T1D progresses and will inform cure research aimed specifically at beta cell preservation.
 Dr. Bruce Verchere (BC) is Professor in UBC Depts of Surgery & Pathology & Laboratory Medicine and Head of the Diabetes Research Program at BC Children’s Hospital Research Institute. He is a world expert in diabetes and islet cell biology, and holds a JDRF grant focused on developing a biomarker to better predict T1D, its progression, and response to therapy. As there is currently no easy way to measure how beta cells are working in people with T1D, this work has the potential to have a major impact on future trials of new T1D treatments.
Dr. Bruce Verchere (BC) is Professor in UBC Depts of Surgery & Pathology & Laboratory Medicine and Head of the Diabetes Research Program at BC Children’s Hospital Research Institute. He is a world expert in diabetes and islet cell biology, and holds a JDRF grant focused on developing a biomarker to better predict T1D, its progression, and response to therapy. As there is currently no easy way to measure how beta cells are working in people with T1D, this work has the potential to have a major impact on future trials of new T1D treatments.
 Dr. Diane Wherrett (ON) is a physician in the Division of Endocrinology, Department of Paediatrics at SickKids and a professor at the University of Toronto. She is the Canadian Centre Director for T1D TrialNet (the international network for risk screening for relatives of people with T1D and preventative clinical trials). Dr. Wherrett leads the CIHR-JDRF Type 1 Diabetes Screening Research Consortium (2023-2028) which will investigate the feasibility of T1D screening in the general population in Canada. The consortium is made up of over 30 members including academic and clinician researchers, people with lived experience of T1D, and knowledge users including a diabetes nurse, genetics counsellor, and a Ministry of Health representative. The acceptability of T1D screening in Indigenous communities will be explored, as led by Indigenous people with lived experience. This research will determine best practices for general population screening for T1D risk and conduct pilot studies of approaches to inform future implementation across Canada.
Dr. Diane Wherrett (ON) is a physician in the Division of Endocrinology, Department of Paediatrics at SickKids and a professor at the University of Toronto. She is the Canadian Centre Director for T1D TrialNet (the international network for risk screening for relatives of people with T1D and preventative clinical trials). Dr. Wherrett leads the CIHR-JDRF Type 1 Diabetes Screening Research Consortium (2023-2028) which will investigate the feasibility of T1D screening in the general population in Canada. The consortium is made up of over 30 members including academic and clinician researchers, people with lived experience of T1D, and knowledge users including a diabetes nurse, genetics counsellor, and a Ministry of Health representative. The acceptability of T1D screening in Indigenous communities will be explored, as led by Indigenous people with lived experience. This research will determine best practices for general population screening for T1D risk and conduct pilot studies of approaches to inform future implementation across Canada.
 Dr. Xiao Yu (Shirley) Wu is a professor at the University of Toronto in the Leslie Dan Faculty of Pharmacy. Her research focuses on the use of nanoparticles to develop novel drug delivery systems and treatment modalities. Nanoparticles are ultrafine particles designed to overcome the limitations of biological barriers and deliver drugs to individual cells. Her JDRF-funded grant will develop a new nanocarrier that can deliver drugs to target islet cells to restore damaged beta cells.
Dr. Xiao Yu (Shirley) Wu is a professor at the University of Toronto in the Leslie Dan Faculty of Pharmacy. Her research focuses on the use of nanoparticles to develop novel drug delivery systems and treatment modalities. Nanoparticles are ultrafine particles designed to overcome the limitations of biological barriers and deliver drugs to individual cells. Her JDRF-funded grant will develop a new nanocarrier that can deliver drugs to target islet cells to restore damaged beta cells.
Dr. Andrew Pepper talks about the cell therapy research he’s working on to make islet transplantation more universal and accessible.
Improving Lives
 Dr. Shazhan Amed (BC) is a clinical professor at UBC and a pediatric endocrinology at BC Children’s Hospital. Her research involves the treatment and prevention of childhood obesity and diabetes. She is particularly interested in developing and evaluating innovative ways to provide the health services necessary for children with diabetes in order to optimize their care and prevent long term complications of this disease. Her JDRF-funded research will establish a paediatric diabetes digital health tool and registry in Canada. Her team will partner with patients, families, and health care professionals to jointly design TrustSphere, a collaborative care experience that will provide individualized clinical care to children and youth with T1D.
Dr. Shazhan Amed (BC) is a clinical professor at UBC and a pediatric endocrinology at BC Children’s Hospital. Her research involves the treatment and prevention of childhood obesity and diabetes. She is particularly interested in developing and evaluating innovative ways to provide the health services necessary for children with diabetes in order to optimize their care and prevent long term complications of this disease. Her JDRF-funded research will establish a paediatric diabetes digital health tool and registry in Canada. Her team will partner with patients, families, and health care professionals to jointly design TrustSphere, a collaborative care experience that will provide individualized clinical care to children and youth with T1D.
 Dr. Gillian Booth (ON), a JDRF-funded scientist at the Centre for Urban Health Solutions within the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto, and a team of researchers are aiming to improve glucose control and patient experiences by using a newly developed virtual care approach to optimize the way health care is delivered to people with T1D.
Dr. Gillian Booth (ON), a JDRF-funded scientist at the Centre for Urban Health Solutions within the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto, and a team of researchers are aiming to improve glucose control and patient experiences by using a newly developed virtual care approach to optimize the way health care is delivered to people with T1D.
 Dr. Sonia Butalia (AB) is a clinician-scientist in the Departments of Medicine and Community Health Sciences at the University of Calgary. Her JDRF-funded project focuses on the transition from pediatric to adult diabetes care, a particularly challenging time for many young people with T1D. Her team will implement a transition program across 5 sites in Alberta that uses non-medical transition coordinator and technology-based communications and evaluate the success of the program and its impact on mental health outcomes. The team will also create an online training plan for other communities across Canada to adopt this transition program.
Dr. Sonia Butalia (AB) is a clinician-scientist in the Departments of Medicine and Community Health Sciences at the University of Calgary. Her JDRF-funded project focuses on the transition from pediatric to adult diabetes care, a particularly challenging time for many young people with T1D. Her team will implement a transition program across 5 sites in Alberta that uses non-medical transition coordinator and technology-based communications and evaluate the success of the program and its impact on mental health outcomes. The team will also create an online training plan for other communities across Canada to adopt this transition program.
 Dr. Deborah Da Costa (QC) is an associate professor in the Department of Medicine at McGill University, scientist at the Research Institute of the McGill University Health Centre, and psychologist at the McGill Comprehensive Health Improvement Program. She previously developed a successful intervention for mental health support during the stages of pregnancy planning, pregnancy, and postpartum. She will now lead a patient-oriented team to redesign the program for people with T1D and T2D, and evaluate its impact on mental health outcomes, ultimately providing opportunities to improve quality of life for women with diabetes during an important life stage.
Dr. Deborah Da Costa (QC) is an associate professor in the Department of Medicine at McGill University, scientist at the Research Institute of the McGill University Health Centre, and psychologist at the McGill Comprehensive Health Improvement Program. She previously developed a successful intervention for mental health support during the stages of pregnancy planning, pregnancy, and postpartum. She will now lead a patient-oriented team to redesign the program for people with T1D and T2D, and evaluate its impact on mental health outcomes, ultimately providing opportunities to improve quality of life for women with diabetes during an important life stage.
 Dr. Ahmad Haidar (QC) is an assistant professor in the Department of Biomedical Engineering at McGill University. Along with his research team and clinical collaborators, he is conducting clinical trials to test whether a novel dual-hormone (insulin and pramlintide) artificial pancreas can eliminate carb counting and lead to easier management of T1D.
Dr. Ahmad Haidar (QC) is an assistant professor in the Department of Biomedical Engineering at McGill University. Along with his research team and clinical collaborators, he is conducting clinical trials to test whether a novel dual-hormone (insulin and pramlintide) artificial pancreas can eliminate carb counting and lead to easier management of T1D.
 Dr. Sylvie Lesage (QC) is a professor at the Université de Montréal and investigator at the Maisonneuve-Rosemont Hospital in Quebec. Dr. Lesage’s laboratory focusses on the genetics of immune system cell populations. Her current work examines the genetic component of pancreatic insufficiency – a lack of enzymes necessary for digesting certain foods – on blood glucose management in T1D.
Dr. Sylvie Lesage (QC) is a professor at the Université de Montréal and investigator at the Maisonneuve-Rosemont Hospital in Quebec. Dr. Lesage’s laboratory focusses on the genetics of immune system cell populations. Her current work examines the genetic component of pancreatic insufficiency – a lack of enzymes necessary for digesting certain foods – on blood glucose management in T1D.
 Dr. Rémi Rabasa-Lhoret (QC) is an endocrinologist and Vice President, Clinic and Clinical Research and a Professor at the Université de Montréal. at Dr Rabasa-Lhoret and his team hold a CIHR-JDRF grant that has enabled support of the BETTER study, which has established a registry of people living with T1D in Quebec, created a virtual education module aimed at improved prevention and management of hypoglycemia, and run multiple small trials focused on improving hypoglycemia outcomes
Dr. Rémi Rabasa-Lhoret (QC) is an endocrinologist and Vice President, Clinic and Clinical Research and a Professor at the Université de Montréal. at Dr Rabasa-Lhoret and his team hold a CIHR-JDRF grant that has enabled support of the BETTER study, which has established a registry of people living with T1D in Quebec, created a virtual education module aimed at improved prevention and management of hypoglycemia, and run multiple small trials focused on improving hypoglycemia outcomes
 Dr. Farid Mahmud (ON) is a staff physician in the Department of Endocrinology at The Hospital for Sick Children and an associate professor of pediatrics at the University of Toronto. He is leading a clinical trial called ATTEMPT that is testing the ability of dapagliflozin, a glucose-lowering drug usually used in type 2 diabetes, to improve glucose control and reduce future risk of complications in teenagers with T1D. In addition, his research examines the impact of diversity (genetics, race, sex, gender, income, family support, etc.) on diabetes management in youth. Using artificial intelligence, his team aims to create a tool for individualized treatment strategies that take into account patient diversity.
Dr. Farid Mahmud (ON) is a staff physician in the Department of Endocrinology at The Hospital for Sick Children and an associate professor of pediatrics at the University of Toronto. He is leading a clinical trial called ATTEMPT that is testing the ability of dapagliflozin, a glucose-lowering drug usually used in type 2 diabetes, to improve glucose control and reduce future risk of complications in teenagers with T1D. In addition, his research examines the impact of diversity (genetics, race, sex, gender, income, family support, etc.) on diabetes management in youth. Using artificial intelligence, his team aims to create a tool for individualized treatment strategies that take into account patient diversity.
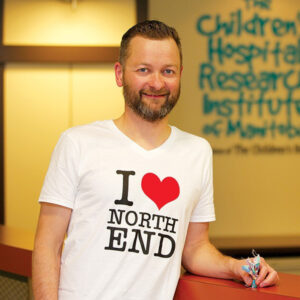 Dr. Jon McGavock (MB) is a professor of pediatrics and child health at the Max Rady College of Medicine at the University of Manitoba and a researcher with the Children’s Hospital Research Institute of Manitoba. His JDRF-funded project aims to improve the mental health of teenagers living with T1D through mentored exercise programs. He will evaluate the effect of increasing physical activity and peer mentorship on diabetes distress and diabetes outcomes.
Dr. Jon McGavock (MB) is a professor of pediatrics and child health at the Max Rady College of Medicine at the University of Manitoba and a researcher with the Children’s Hospital Research Institute of Manitoba. His JDRF-funded project aims to improve the mental health of teenagers living with T1D through mentored exercise programs. He will evaluate the effect of increasing physical activity and peer mentorship on diabetes distress and diabetes outcomes.
 Dr. Mahla Poudineh (ON) is an assistant professor at the University of Waterloo focusing on biomedical engineering. Dr. Poudineh’s laboratory is developing a new biosensor that will be capable of continuously measuring blood ketones and glucose simultaneously.
Dr. Mahla Poudineh (ON) is an assistant professor at the University of Waterloo focusing on biomedical engineering. Dr. Poudineh’s laboratory is developing a new biosensor that will be capable of continuously measuring blood ketones and glucose simultaneously.
 Dr. Marie-Eve Robinson (ON) is an assistant professor at the University of Ottawa and a pediatric endocrinologist at the Children's Hospital of Eastern Ontario. Dr. Robinson researches the genetics of pediatric disease, while also focusing on the impact of childhood chronic disease on quality of life and psychiatric health. Her recent work is assessing the effectiveness of a mindful self-compassion program on improving diabetes distress in youth with T1D.
Dr. Marie-Eve Robinson (ON) is an assistant professor at the University of Ottawa and a pediatric endocrinologist at the Children's Hospital of Eastern Ontario. Dr. Robinson researches the genetics of pediatric disease, while also focusing on the impact of childhood chronic disease on quality of life and psychiatric health. Her recent work is assessing the effectiveness of a mindful self-compassion program on improving diabetes distress in youth with T1D.
 Dr. Peter Selby (ON) is a clinician scientist at the Centre for Addiction and Mental Health (CAMH) and professor at the University of Toronto. Dr. Selby uses technology to combine clinical medicine and public health methods to scale up and test health interventions. His current work uses technology to deliver a patient-based comprehensive care program to young adults with T1D that are experiencing diabetes distress.
Dr. Peter Selby (ON) is a clinician scientist at the Centre for Addiction and Mental Health (CAMH) and professor at the University of Toronto. Dr. Selby uses technology to combine clinical medicine and public health methods to scale up and test health interventions. His current work uses technology to deliver a patient-based comprehensive care program to young adults with T1D that are experiencing diabetes distress.
 Dr. Tricia Tang (BC) is a clinical psychologist and an associate professor at the University of British Columbia’s Faculty of Medicine. Her work focuses on developing and evaluating low-cost and sustainable models to improve long-term diabetes-related health outcomes in high-risk and medically underserved patient populations. Recently, she was awarded a JDRF grant to work on the implementation of a virtual care platform called REACHOUT designed to improve mental health for people living with T1D in rural and remote regions of BC.
Dr. Tricia Tang (BC) is a clinical psychologist and an associate professor at the University of British Columbia’s Faculty of Medicine. Her work focuses on developing and evaluating low-cost and sustainable models to improve long-term diabetes-related health outcomes in high-risk and medically underserved patient populations. Recently, she was awarded a JDRF grant to work on the implementation of a virtual care platform called REACHOUT designed to improve mental health for people living with T1D in rural and remote regions of BC.
 Dr. Holly Witteman (QC) is the Canada Research Chair in Human-Centred Digital Health and a Full Professor in the Department of Family & Emergency Medicine at Université Laval. With an interdisciplinary background in human factors engineering and social sciences, she is developing CommuniT1D. This will be a virtual platform for peer information and connection in a small group format for people who have things in common. Holly has personally lived with T1D for over 40 years.
Dr. Holly Witteman (QC) is the Canada Research Chair in Human-Centred Digital Health and a Full Professor in the Department of Family & Emergency Medicine at Université Laval. With an interdisciplinary background in human factors engineering and social sciences, she is developing CommuniT1D. This will be a virtual platform for peer information and connection in a small group format for people who have things in common. Holly has personally lived with T1D for over 40 years.
Dr. Tricia Tang discusses the importance of taking care of your mental health as a key component of managing type 1 diabetes.
Helping us navigate our research funding priorities, which are shaping T1D research both in Canada and globally, while communicating the latest updates to our donors, supporters and T1D community is our Chief Scientific Officer, Dr. Sarah Linklater.


