The American Diabetes Assocation’s 83rd Scientific Sessions were held from June 23- 26th. This annual conference brings together researchers and scientists to both present and learn about the latest in type 1 diabetes research and technological advancements. Many of the presenters are funded by JDRF International, JDRF Canada’s affiliate in the United States.
JDRF-funded researchers presented new study results that will improve outcomes for people with diabetes (T1D). Chief Scientific Officer, Dr. Sarah Linklater, was in attendance, along with many Canadian researchers that JDRF donors generously help to fund through the $100 M Campaign to Accelerate. An impressive program was presented including breakthrough clinical trials and significant research studies that are paving the way to novel treatments and technologies for T1D.
You can view all the oral and poster presentations on the Diabetes Journal website.
Updates in Cure-based Research:
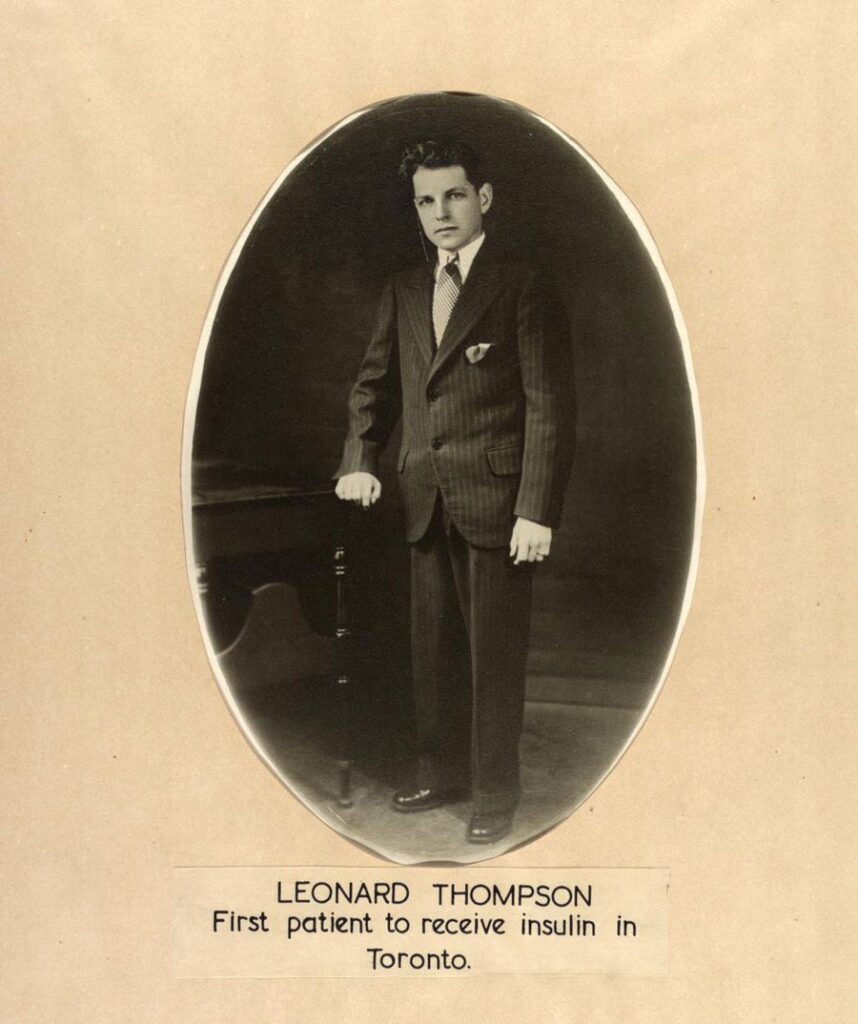
- An update on Vertex’s clinical trial to test VX-880, a stem cell-derived replacement therapy for diabetes, was presented by Trevor Reichman, M.D., Ph.D. (University of Toronto). Data from 6 participants was presented, and the two with more than a year of follow-up no longer need to administer insulin through injections or pump therapy and exceeded the recommended time-in-range for blood glucose. Vertex’s phase I/II clinical trial of VX-880 was made possible by Doug Melton’s years of JDRF-funded research and a catalytic investment from the T1D Fund in Semma Therapeutics—a biotech company founded by Melton to develop a stem cell-derived islet therapy for T1D—which was acquired by Vertex Pharmaceuticals in 2019.
- Vertex is also now recruiting patients in Edmonton for their VX-264 therapy. This treatment will use the same cell therapy as VX-880 but encapsulate the cells within a device designed to shield the cells from the body’s immune system, meaning immunosuppression should not be required.
- In Sernova’s ongoing Phase 1/2 clinical trial of their Cell Pouch System™ – a novel implantable and scalable medical device that forms a natural environment in the body for the housing and long-term survival and function of therapeutic cells – the first five patients to receive the encapsulated donor islet transplants achieved insulin-independence for ongoing periods of six to 38 months. Sernova is a Canadian biotech company headquartered in London, Ontario.
- Dr. Harald Stover, CEO of Allarta Life Sciences Inc (Hamilton, Ontario) presented an update on their work using hydrogel microencapsulation for immunoprotective islet replacement therapy.
- The clinicians and scientists at University of Alberta presented a 20-year follow up on renal function after islet transplant with whole-body immunosuppression. Highlighting the importance of effective and tailored immunosuppression regimens, and the ultimate goal to reduce or eliminate the need for immunosuppression with transplantation.
- Dr. Cristina Nostro, whose work is closely tied and complementary to these trials, shared her excitement in stem cell research, recapping the day’s sessions by saying: “In the last 20 years, we’ve learned how to differentiate these cells, and now we’re moving them to the clinic and they’re giving us the results that we want. The future is bright. I’m super excited, and I hope you are too.”
Updates in Disease-modifying Therapies
- JDRF-funded researchers Halis Akturk, M.D., Martin Thelin, M.D., Ph.D., and Edwin Liu, M.D., presented on the relationship between T1D and other diseases, highlighting how other diseases can be a resource for better understanding and managing T1D.
- Evaluation of a disease-modifying therapy that may delay or prevent the disease, was presented by Farooq Syed, Ph.D., a JDRF career development awardee.\
Updates in Improving Lives:
- Researchers and companies at the conference also reported exciting updates to diabetes devices that are now getting smaller, more coordinated, and more automated while improving glucose control and easing the burden of diabetes management.
- The team behind the BETTER Project in Quebec led by Drs. Anne-Sophie Brazeau and Remi Rhabasa-Lhoret presented multiple research findings including information on clinical characteristics of LADA (latent autoimmune diabetes of the adult), a comparison between DIY and commercialized automated insulin delivery systems, the use of oral glucose at higher thresholds to prevent mild hypoglycemia, the addition of glucagon to insulin administration to reduce post-meal hypoglycemia, and a comparison of injectable versus intranasal glucagon administration.
- A randomized clinical trial, presented by JDRF grantee Schafer Boeder, M.D., showed that a medication that helps lower blood sugar (SGLT) plus a glucagon receptor treatment improved blood-sugar control and reduced insulin dose, and there was no diabetic ketoacidosis (DKA)—a risk when just taking an SGLT treatment for T1D.
- Zucara Therapeutics (a Toronto-based company supported by JDRF) presented the positive results of their Phase 1 trial of ZT-01, a novel therapy to prevent hypoglycemia. Following the success of phase 1, Zucara has recently begun Phase 2 clinical trials to evaluate the efficacy of ZT-01 to prevent nighttime hypoglycemia.
- Dr. Tricia Tang chaired a session that covered research and initiatives that address the psychosocial aspects of T1D. Dr. Tang also reported in her own talk that through her ongoing trial of the peer support app T1DReachout, she’s learned that individuals require peer support that is choice-based, customizable, and “just in time,” meaning peer support provides an emotional lifeline when people need it most.
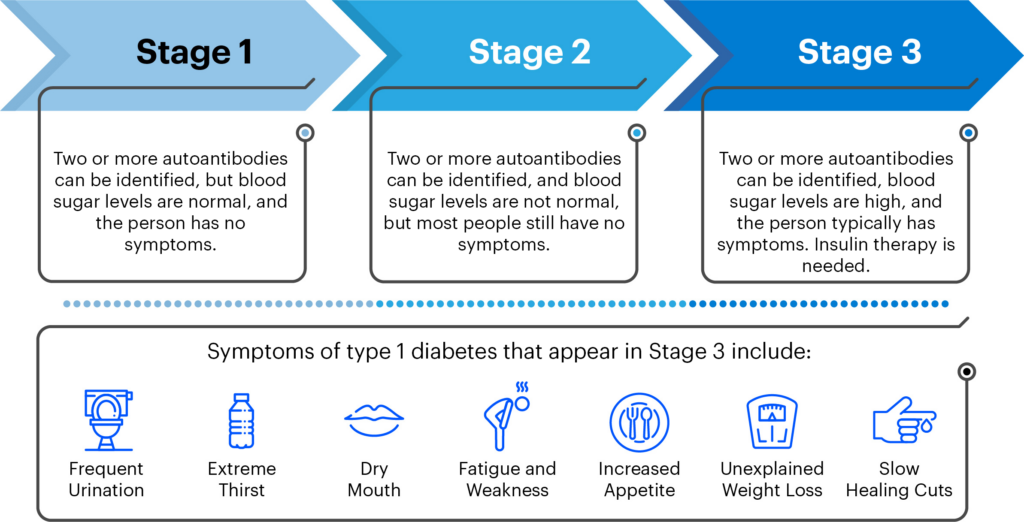
Updates in Screening
- There was a lot of success in T1D screening presented at ADA, including a JDRF-led symposium on the identification and prevention of T1D. These successes will help inform the CIHR-JDRF Screening Research Consortium, being announced on July 10th. This consortium will investigate the best ways to implement a Canada-wide, universal screening program integrated with the Canadian healthcare system.
To learn more about the sessions, please find the recaps for Day 1, Day 2, and Day 3 of the conference.